Braces Covered by Medicaid States: Find Out Which States Offer Coverage
Braces Covered by Medicaid States: Your 2025 Guide to Orthodontic Benefits
Did you learn that it almost entirely depends on your zip code in deciding whether or not your child can have braces with the help of Medicaid? The process of Medicaid coverage of braces is one of the most confusing and daunting issues when it comes to parents and adults who need to get affordable orthodontic services. An analysis conducted by the National Health Policy Institute in 2025 revealed that the Medicaid criteria of braces differ radically across the 50 states, and many families are left in confusion concerning whether they are eligible or not.
This is a sure direction guide. We will unveil the secret, and you will see plainly state-by-state what Medicaid covers to dental braces, the stringent eligibility conditions required of you to be covered, and a realistic step by step action plan to discover what you have to do and where to find Medicaid dentists braces cover. We want to provide you with the information and the resources to effectively go through with this process and find the necessary dental care that you or your child require.
Understanding the Basics: How Medicaid and Orthodontics Work
Medicaid represents a state/ federal collaboration and this is exactly why no single, national response to the question does Medicaid cover braces? The programs are administered by each state in its own way, which causes a patchwork of regulations. But still, there are principles which are common to all states.
The Essential Distinction: Children vs. Adults
This is the most critical factor in determining if you can get braces on Medicaid.
- Regarding Children (Under 21): The Federal law has stipulated that the state Medicaid programs should offer periodic and early screening, diagnostic and treatment (EPSDT) services to children. This implies that they have to pay the entire amount of any health service that is necessary medically and it can also involve orthodontics such as braces provided that a set of requirements are satisfied. It is not a certain advantage, but a possible one.
- In the Adults (21+): States are not obliged to offer dental benefits to adults. Adult braces are extremely unavailable in Medicaid and usually reserved in very few cases, including when the disabled are considered on certain waiver programs or after a major trauma.
What Does “Medically Necessary” Actually Mean?
There is no Medicaid coverage of braces due to cosmetic purposes. The inquiry is what type of braces are covered by Medicaid. is secondary to why does Medicaid cover braces? Only severe, functionally impairing conditions are generally covered, with a number of them usually being indexed.
The most frequently utilized one is the Handicapping Labialingual Deviation (HLD) Index. The orthodontist of your child will assess the grade of the malocclusion (bite problem) with this index. Different states have different passing cut-off scores. Some of the common conditions that can be qualified include:
- Severe overjet (sticking out front teeth) which are highly prone to getting traumatized.
- Cleft palate and other craniofacial defects.
- Extreme crowding which makes it difficult to eat or speak.
- Severe underbites or crossbites, which lead to dysfunction of the jaw.
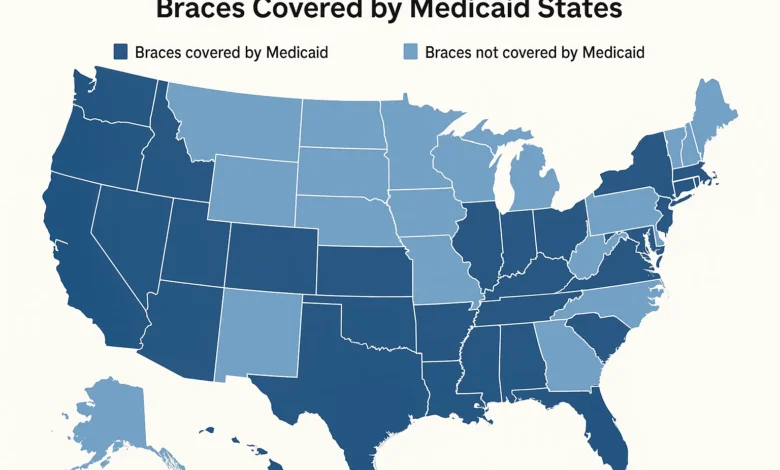
State-by-State Breakdown: Where Are Braces Covered by Medicaid?
The table below gives a broad summary of the Medicaid landscape affecting the braces among children. This data is not permanent and you should continuously need to confirm with your individual state Medicaid managed care plan.
Medicaid Orthodontic Coverage by State (Children)
| Coverage Level | Description & Common HLD Cut-off Score | Example States |
|---|---|---|
| Comprehensive | Coverage is available for a wider range of cases. HLD cut-off scores may be lower (e.g., 26 points). | California, New York, Illinois, Massachusetts, Washington |
| Limited/Restrictive | Coverage is only for the most severe, handicapping conditions. High HLD cut-off scores (e.g., 30+ points). | Texas, Florida, Georgia, Arizona, North Carolina |
| Emergency Only | Routine orthodontics is not covered. Only treatment for acute pain or trauma-related issues. | Alabama, Mississippi, Tennessee* |
*Note: States marked with an asterisk may have limited programs or waivers. This is a generalized guide. For example, Tennessee’s TennCare program has historically had very limited orthodontic benefits.
Key States in Detail
California (Medi-Cal)
California has had one of the more detailed orthodontic programs. It is based on the HLD index and children with the required score level are covered by the programs such as Denti-Cal. The state has also a greater braces place network around me that accepts Medicaid.
Texas (TMHP)
The use of Texas Medicaid on orthodontics came into headlines previously because of fraud issues, and much stricter rules were put in place. In modern times, the approval is extremely limited and limited to the case of the most severe cases. The HLD score requirement is also one of the highest in the country.
New York (NY Medicaid)
New York offers fairly strong orthodontic coverage to children with medical necessity. This will always need prior authorization and the process may be very time consuming but the coverage is available.
Florida (Sunshine Health, etc.)
Similar to Texas, Florida is also very demanding with regard to the required score in HLD, thus hard to qualify. The most functionally impairing conditions only are covered.
Pro Tip: Do not rely solely on this table. The most important question to ask your state or managed care plan is: “What Medicaid insurance covers braces under my specific plan, and what is the current HLD index cut-off score for prior authorization?”
The Step-by-Step Guide to Securing Medicaid Braces
Knowing which states Medicaid cover braces is step one. Now, here is your 5-step action plan to navigate the process successfully.
- Check Your Eligibility and Plan: To begin with, check whether your child is enrolled actively in the Medicaid. Next, find out what managed care do you have (e.g., Molina, UnitedHealthcare, Aetna Better Health). The first area to look in your plan is the members handbook where there are dental benefits. Dial the number on the back of your card and request specifically: Does my plan include orthodontics among children and what are the conditions?
- Locate a Participating Provider: This is the step that cannot be neglected. You need to get a dentist that is under your individual Medicaid plan. Go to the online provider directory of your plan and type in the word orthodontist or pediatric dentist. Another way is to place local calls and enquire, “Will you provide orthodontic services to [Your Plan Name] Medicaid? This is the response to the query of braces that accept Medicaid.
- Make an Appointment: Have the orthodontist make appointment with the in-network orthodontist. On this visit, it is necessary to be open and tell them that you are requesting treatment on the Medicaid. The orthodontist will do a detailed examination, provide X-rays and models, and complete the scoring of the state of the child by using the HLD index.
- Complete the Prior Authorization Process: The office of the orthodontist will have prepared an elaborate treatment plan which will include the HLD score and clinical evidence (photos, X-rays) to your Medicaid plan to get a go-ahead. This is the most fundamental stage. Treatment should not be started before you have been issued with an Approval Letter by Medicaid.
- Know Your Financial Obligation: Although it is approved, inquire about any possible out of pocket expenses. Although in most cases Medicaid pays the full amount of the approved services, there are possibilities of co-payments in some of the visits or in certain situations. Always get it in writing.
Special Considerations: Adults, Types of Braces, and Appeals
What About Adult Braces on Medicaid?
The query is; is Medicaid used to cover adult braces? has itself a short but noteworthy reply: Almost never. Orthodontic coverage of adults is very uncommon since states are not mandated to offer dental benefits to the adults. Exceptions might include:
- Medicaid beneficiaries aged, blind, and disabled with a defining qualifying condition.
- The family obtains treatment after a recorded accident that necessitated the work of an orthodontist to fix an operation.
- Patients who have some medically intricate conditions such as cleft palate.
When you are an adult and you want to have braces under Medicaid, then the first step would be to call the Medicaid office in your state and enquire whether there are any such exceptions.
What Types of Braces Are Covered?
Do traditional metal braces qualify as the type of braces that Medicaid covers? The answer, as usual is almost always yes. Coverage of clear aligners such as Invisalign is highly unlikely to be financed through Medicaid since it is usually regarded as a cosmetic option and it is pricier. Medicaid orthodontics aims at seeking to correct the medical issue in the most economic way.
What to Do If You Are Denied
Denials are common. Do not give up. You have the right to appeal. The denial letter will contain the instructions of the filing of an appeal. Gather more evidence, such as more photos, a letter of medical necessity, or second opinion, with your orthodontist so that they can be more helpful during the process of appeals.
Underbite Correction Jaw Surgery: What to Expect Before & After
Frequently Asked Questions (FAQ)
Does Medicaid fully cover braces?
In case the treatment is pre-determined and approved, the Medicaid usually pays a 100 percent of the cost, in-network providers. Nevertheless, this should always be verified with your particular managed care plan with certain ones having nominal co-pays.
Where would I get Medicaid-accepting braces?
Find a Provider is the most dependable tool that should be utilized on the site of your particular Medicaid managed care. Another way of checking is to call the local orthodontic offices and inquire whether they are taking new Medicaid patients of the orthodontics under your name as the plan.
Are the adults insured by the state through braces?
In most cases, no. State Medicaid programs do not require dental or orthodontics of adults. Medicaid has a limited number of very specific medical situations that are covered under adult braces.
Why is the denial of braces by Medicaid the most frequent?
The most frequent denial is that the condition of the patient did not receive a high rating on the index of orthodontic need required by the state (such as the HLD) to be considered as medically necessary. The case is not functional but cosmetic.
Is KoolAid compatible with Medicaid?
It is highly unlikely. In Medicaid, traditional metal braces are almost the only standard of care available to be treated economically. Clear aligner systems are hardly, or not at all covered.
What is the amount of income to qualify to have Medicaid braces?
Braces have no distinct income limit. To obtain Medicaid, you have to individually meet the state-based income and household size requirements of children (e.g., CHIP or MAGI-based eligibility). In case you are enrolled then you have to satisfy the additional medical necessity requirements of orthodontics.
Conclusion: Your Path to a Healthier Smile
Striking a balance between the world of braces paid by Medicaid states is not an easy task to perform, but it is not the only one. The main conclusions are obvious: the coverage is mostly aimed to children with medically necessary conditions, the regulations in each state are very different, and your possibility to succeed depends on the careful procedure of verification, finding an in-network provider, and prior authorization.
Although the journey of the adults is much more restricted, the knowledge of the system is the initial step to ensuring your family is healthy. No one should think that you are not eligible. Be active, tenacious and utilize the resources that have been discussed in this guide.
Your second action: Take up the phone. Call the member services number of your Medicaid card and inquire the critical questions regarding the benefits of orthodontics. Then, you use online directory of your plan so that you can begin to search a qualified, participating orthodontist. It is that first informed phone call that starts you on your path to a healthier functional smile.



