Expander Covered by Medicaid – Find Out If You Qualify
Is an Expander Covered by Medicaid? Your Complete Guide to Orthodontic Benefits
Understanding Medicaid: Traditional vs. Expansion Programs
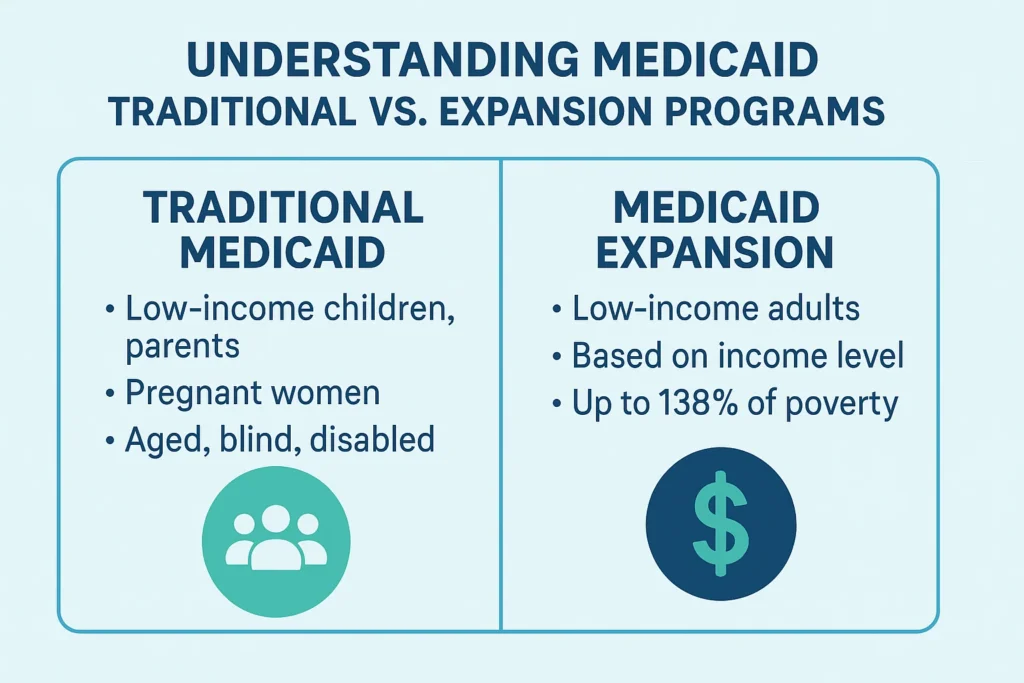
Before we dive into orthodontics, it’s crucial to understand the two main types of Medicaid, as this forms the foundation of all coverage, including whether a palate expander is covered by Medicaid.
What is Traditional Medicaid?
Traditional Medicaid, as it is commonly known as the fee-for-service Medicaid, covers certain group of low-income citizens including children, pregnant women, parents/caretakers, the elderly, and individuals with disabilities. The federal government mandates coverage but provides it through states and thus, it is highly varied.
What is Medicaid Expansion under the ACA?
The Affordable Care Act (ACA) allowed states to expand Medicaid coverage to nearly all low-income adults under the age of 65 with incomes up to 138% of the federal poverty level. This is known as adult expansion medicaid. By 2024, the expansion has been adopted in 40 states and Washington D.C. The benefits provided through the expansion plans are usually not the same as the traditional Medicaid especially in the case of the adult covering on dental and orthodontic benefits.
Key Takeaway: The type of Medicaid plan you have—traditional or expansion—is the single biggest factor determining your coverage for orthodontic appliances like expanders.
Medicaid Orthodontic Coverage for Children: The EPSDT Mandate
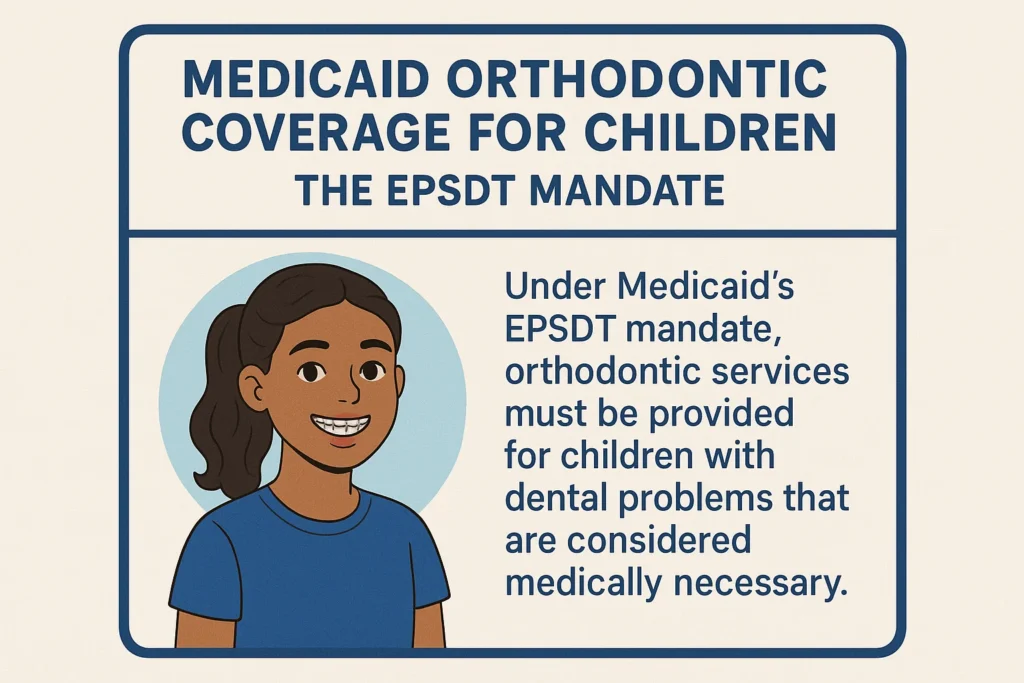
In children (under 21), the coverage is much stronger due to a federal requirement known as Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) benefit. EPSDT mandates state Medicaid programs to reimburse any service, which is medically necessary so as to remedy or alleviate defects and bodily and mental illness and conditions, which are found during a screening.
This implies that when a licensed orthodontist is found to have a condition such as a severely narrow palate, a crossbite, or a lot of crowding that affects the child function or health, the Medicaid has been legally mandated to pay the mandated treatment, which may be a palate expander.
What Does “Medically Necessary” Mean for an Expander?
Medicaid will not cover expanders for purely cosmetic reasons. “Medically necessary” typically means the condition:
- Impairs eating or chewing: Difficulty biting or chewing food properly.
- Causes sleep apnea or breathing issues: A narrow palate can contribute to airway obstruction.
- Results in speech impediments: Affecting the ability to form sounds correctly.
- Causes TMJ pain or jaw dysfunction: Leading to chronic pain or headaches.
- Creates a high risk of tooth decay or gum disease: Due to severe crowding that makes cleaning teeth impossible.
Adult Medicaid Coverage for Expanders: A Different Story
The adult environment is completely different. Medicaid is not mandated to cover dental benefits, not to mention orthodontics, to people above 21. The coverage is completely at the will of the state.
- Classical Medicaid among Adults: The dental benefits among the adults in most non-expansion states are either highly restricted or not present at all. Expanders and other forms of orthodontic care such as expanders among adults is extremely unavailable and is normally only covered under severe trauma or congenital disability.
- Adult Expansion Medicaid Coverage: States that expanded Medicaid under the ACA must offer essential health benefits, including dental care of children but not adults. Most expansion states, however, decide to include some limited benefits of adults in their expansion plan. Even in that case, complete orthodontics is practically not factored in.
State-by-State Variability in Medicaid Expansion Coverage
Since Medicaid is state based, orthodontics, with expanders included, are covered in an uneven manner. California might have what Texas does not cover. A brief generalized examination of the orthodontic coverage environment of children is presented in the table below.
| State Category | Typical Orthodontic Coverage for Children | Example States |
|---|---|---|
| Comprehensive Coverage | Coverage for medically necessary expanders and braces is common if strict criteria are met. | California, New York, Massachusetts, Washington |
| Limited Coverage | Coverage may be available but with extremely restrictive criteria, often only for the most severe cases. | Florida, Arizona, Michigan, Georgia |
| Minimal to No Coverage | Routine orthodontics is rarely covered. Coverage may only be available through a managed care plan or waiver program. | Alabama, Mississippi, Tennessee* |
*This is a generalization. You must check with your specific state’s Medicaid program or managed care organization for exact benefits.
5-Step Action Plan to Get Your Expander Covered by Medicaid
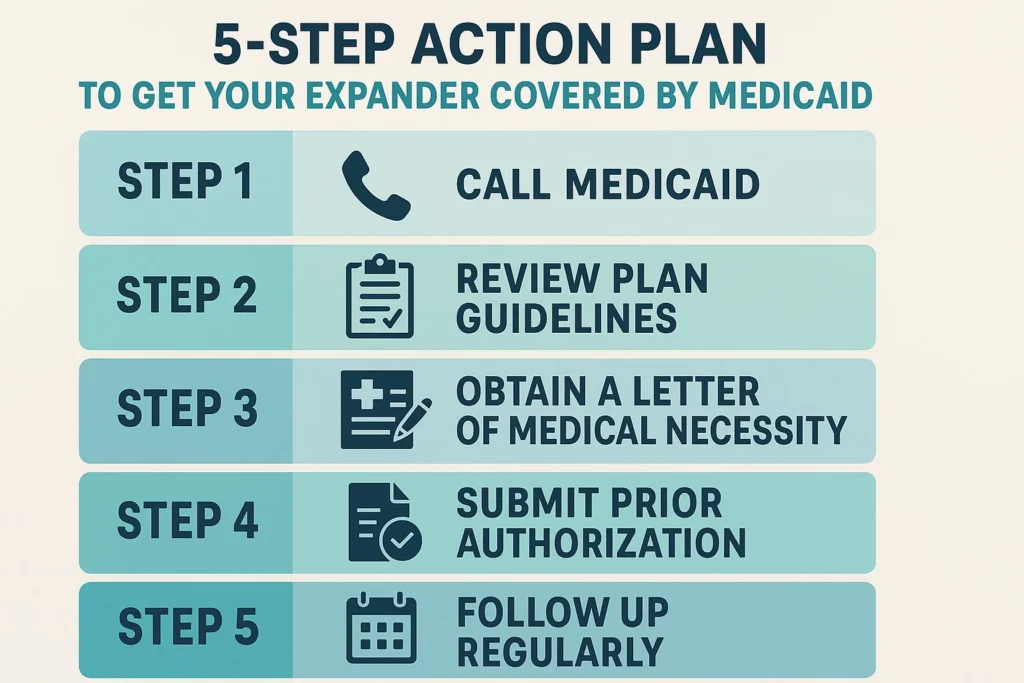
- Check Your Eligibility and Type of plan: Visit the Medicaid portal of your state, or dial the member services number of your card. Make sure that you have either traditional Medicaid or an expansion plan and ask to be provided with a summary of dental and orthodontic benefits.
- Make an appointment with a Dentist: The first thing you have to do is a visit to a dentist that takes Medicaid. They are able to carry out primary examination and refer to an orthodontist in case of necessity.
- Locate an Orthodontist that takes Medicaid: This is of the essence. The orthodontists do not all take part in the Medicaid program. One of them can be found in your plan provider directory. Pro-Tip: When you make an appointment with the orthodontist call their office to be sure they take on new patients with Medicaid.
- Get a Comprehensive Orthodontic Examination: The orthodontist will provide an extensive examination, X-rays, and pictures and establish whether or not an expander is medically necessary. They will record the way the condition fulfills the medical necessity requirements of your state.
- Send a Pre-authorization: The office of the orthodontist will do this. All clinical documentation, photos, and X-rays will be presented to the Medicaid by them. You do not continue the treatment unless you are given an approval letter in writing.
Frequently Asked Questions (FAQ)
Is dental included in Medicaid expansion among adults?
What is the distinction between a spacer and an expander? Are spacers Medicaid covered?
Who qualifies in Medicaid expansion?
What should I do with the expander of my child, denied?
Does orthognathic (jaw) surgery come under the Medicaid?
Conclusion: Empowering Yourself to Access Care
Navigating whether an expander is covered by Medicaid can feel overwhelming, but understanding the system is the first step to advocacy. In the case of children, the EPSDT benefit will offer a close gateway to medically indispensable orthodontic services. In case of adults, there are much less opportunities and strongly dependent on the policies of your state. Verification, documentation and perseverance is the key to success. Check your benefits, have a dentist that is in Medicaid and make sure they document the necessity of the medical treatment meticulously.
Your next step: Don’t operate on assumptions. Call your managed care plan or state medicaid office today and have the phone. Request your own dental benefits book. This is all that you need to clear your head and move on.
Expander Side Effects Orthodontics: The Truth About Pain & How to Cope